
Malignant lymphomas are among the tumors that are highly sensitive to radiation therapy. Radiation therapy is usually recommended as an adjunctive treatment after previous systemic treatment (chemotherapy, biological treatment). It is usually targeted at the areas with the highest risk of failure (original tumor sites, large tumors). Due to the excellent effectiveness of radiotherapy (RT), it is not necessary to use radiation doses that exceed the tolerance limits of the surrounding tissues. The problem of irradiating malignant lymphomas lies in most cases in reducing the dose to the surrounding organs at risk. From a long-term perspective, patients after RT are particularly at risk of developing secondary malignancies and cardiovascular diseases. You can read more about RT for lymphomas in the article Radiotherapy in the Treatment of Lymphomas (bulletin LymfomHelp).
14 studies confirmed that proton RT significantly reduces the radiation exposure to high-risk organs. Proton RT should therefore be considered in selected patients in whom it is able to significantly reduce doses to risk structures.
PTC focuses primarily on high-risk groups where the benefits of proton therapy are highest and well established. These are:
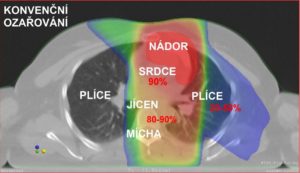
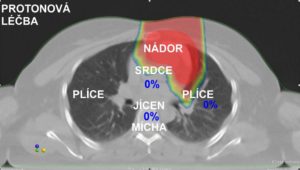
Picture of the photon and proton plan, where you can see the dose distribution for individual organs.
A large group of lymphoma patients indicated for RT are those with a very good long-term prognosis. These patients should be treated with awareness of the long-term risks of cancer therapy. This includes especially young patients with Hodgkin’s lymphoma and prognostically favorable B-cell non-Hodgkin’s lymphoma (especially aggressive subtypes of diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma). The “dose limiting” approach should not be used for these patients, rather the least burdensome RT technique should always be considered. Proton therapy for the mediastinum offers the greatest benefits. In 2018, the International Lymphoma Radiation Oncology Group (ILROG) recommendation for proton RT in adults with mediastinal lymphoma localization was published: http://www.bloodjournal.org/content/132/16/1635?sso-checked=true
Patients who have the maximum benefit from proton RT were identified in this study.
A smaller group consists of patients with refractory or relapsing lymphomas with localized involvement, most often with a large finding in the mediastinum: https://www.redjournal.org/article/S0360-3016(17)31205-1/fulltext
Due to the greater aggressiveness of the disease, it is necessary to increase the total radiation dose and standard photon RT is burdened with a high risk of post-radiation complications. Proton RT can be used in this situation as a separate curative method or as “debulking” (reduction of tumor mass) before planned systemic treatment (such as allogeneic transplantation). For some patients, proton RT may be part of a curative treatment approach in situations that were previously considered “incurable”.
In a similar indication, we can recommend proton RT for repeated irradiation, when the organs at risk are already burdened with a dose from the previous RT. Even here, with limited disability, it is possible to achieve long-term control of the disease.
Link: (Hull MC, Morris CG, Pepine CJ et al. Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of hodgkin lymphoma treated with radiation therapy. JAMA. 2003; 290 (21): 2831-7. (Cellai E, Magrini SM, Masala G, et al., The risk of second malignant tumors and its consequences for the presentation: analysis of a series pf 1524 cases consecutively treated at the Florence University Hospital. Int J Radiat Oncol Biol. Phys. 2001;49(5): 1327-37). https://pubmed.ncbi.nlm.nih.gov/14657067/.
Purchase the book via the link below.
Purchase the book via the link below.